What is the dirty little secret of drugs for lifestyle diseases?
To avoid getting in the way of consumer advertising, for example, consumer advertising, pharmaceutical companies “disclose medicines as a solution that prioritizes cholesterol management while underestimating lifestyle changes.” Like the editors of the American Medical Association’s magazines, this is reflected in the medical literature. “Despite decades of recommendation for improvement, the high prevalence of poor lifestyle behaviors leading to increased risk factors for cardiovascular disease has allowed myocardial infarction (heart attack) and stroke to continue to be the leading cause of the United States.” Do we really need to drug more people? A response has been published in a British medical journal. “Once again, the doctor is begged to get “real.” We hope that efforts to help patients and communities adopt healthy lifestyle habits will be successful and that more statin prescriptions will begin. Cholesterol-lowering agents that earn billions of dollars per year on annual sales.
Every time cholesterol guidelines expand the number of people eligible for statins, they are accused of “a big kiss to the big pharma.” This is understandable as most of the members of the guidelines panel were “industry-related.” However, these days, there are cheaper generic versions, as all major statins are not present. For example, the safest and most effective statin is the common Lipitor, which is sold only a few dollars a month as atorvastatin. So these days, cholesterol guidelines are not necessarily “part of the industry’s conspiracy.”
“The way of life in the United States is a problem, not a guideline…” The reason so many people are candidates for cholesterol and blood pressure lowering medication is because so many people take such awful care. The bottom line is that “individuals must take more responsibility for their health behavior.” What if you are reluctant to improve your diet and make lifestyle changes to reduce the risk, or if it is not possible? If your 10-year risk of having a heart attack is 7.5% or more and stays like that, the benefits of taking statin medications can outweigh the risks. But that’s really what you decide. It’s your body, your choice.
“Whether the overall benefits balance justifies the use of an individual patient’s medication cannot be determined by the guidelines committee, the health system, or even the attending physician. Instead, it is the individual patient who has the fundamental right to determine whether it is worth taking the drug.” This was recognized by some of the medical “hippocratics and other historical figures,” but “in recent decades, medical professionals have begun to move from paternal “doctors know best” stances to those who explicitly support patient-centered evidence-based shared decision-making. “One of the problems in communicating evidence of statins to support this shared decision-making is that most physicians “do not understand the concept of risk and probability, and their further exposure to undergraduate and graduate education statistics, makes little difference.” However, that understanding is important for preventive medicine. When doctors provide cholesterol-lowering medications, they do something completely different from treating patients who have asked for help because they are sick. They are not as doctors as life insurance salespeople, and are pitching postponed benefits in exchange for small (but not ignored) continuous inconveniences and continued inconveniences and costs with this new kind of medication. Dive in and see exactly what is at risk.
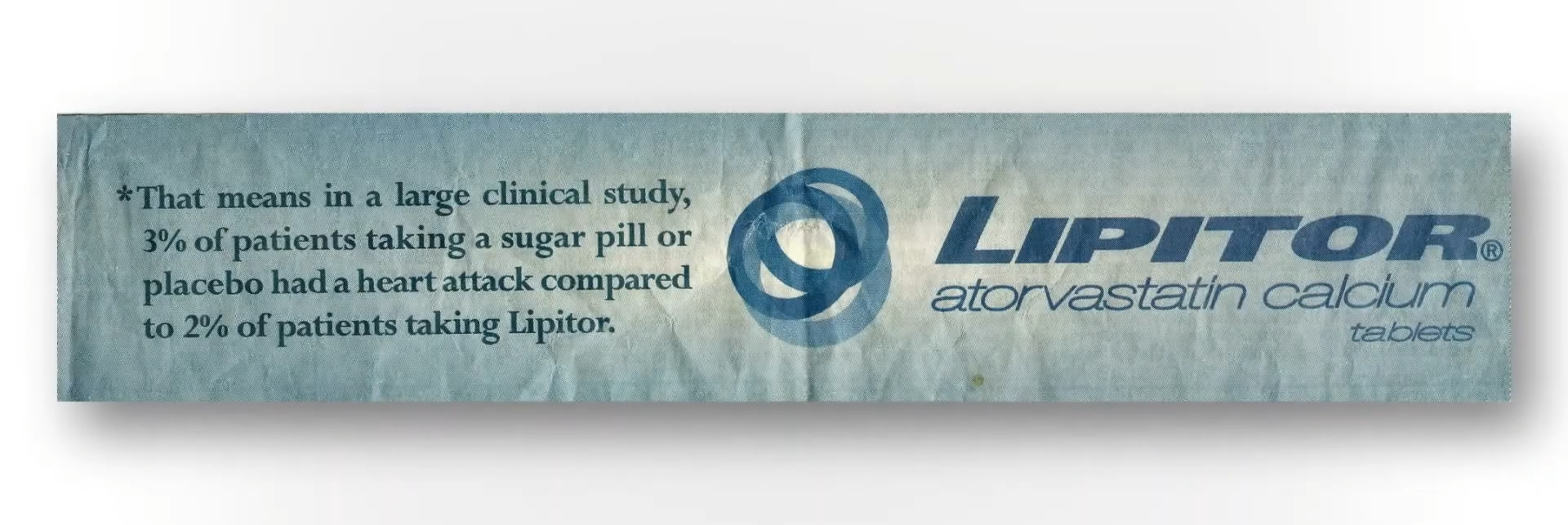
Do you have a doctor in my video that misleads patients about the risks and benefits of statins below and at 3:55? This is a Lipitor advertisement. When pharmaceutical companies say statins reduce the risk of a heart attack by 36%, that’s the relative risk.
If you follow the asterisk that I swirled after “36%” in the ad, you can see how they came up with it. I included it here in my video at 3:56. In a large clinical study, 3% of patients who were not taking statins had a heart attack within a certain period of time, compared to 2% of patients who took the medication. Therefore, this drug dropped the risk of a heart attack from 3% to 2%. This is about a third of decline, so 36% reduced their relative risk statistics. However, another way to see it going from 3% to 2% is that the absolute risk was reduced by only 1%. So, in reality, “The chance to avoid a fatty heart attack over the next two years is around 97% without treatment, but can be increased to about 98% by taking crest (statin) every day.” Put another way, 100 people have to be treated with drugs to prevent a single heart attack. That statistics may shock many people.
When asked what patients were led to believe, they don’t think they have one in 100 chances to avoid a heart attack within a few years with statins, but they do not think they are one in two. Not only 1% of patients, but most patients. And this “disparity between actual and expected effects can be viewed as a dilemma. On the other hand, it is ethically unacceptable for caregivers to intentionally support and maintain the expectations of fantastic treatment by patients.” We cannot mislead people to think that drugs work better than they actually are, but on the other hand, how else do we make people take the medication?
When asked, people want an absolute risk reduction of at least about 30% to take cholesterol-lowering medications every day, but the actual absolute risk reduction is only about 1%. So the dirty little secret is that if the patient knew the truth about how it wasn’t actually working, no one would agree to take them. Doctors are not educating their patients or are not actively misinforming them. Given that the majority of patients expect much greater benefits than they can get from statins, they learn the truth: “There is a tension between patients’ rights to know about benefiting from preventive medications and when they are so informed, there is a tension between reduced intake (the willingness to take the drug). This sounds terribly paternal, but it could potentially put hundreds of thousands of lives at risk.
People will die if the patients were fully informed. Approximately 20 million Americans use statins. Even if the drug saves a hundredths of the time, if everyone stops taking statins, it could mean hundreds of thousands of lives will be lost. “It’s ironic that notifying patients about statins increases the very outcomes they’ve designed to prevent.”





