How do I calculate my personal risk of heart disease to determine if I need to start a cholesterol-lowering statin medication?
Muscle-related side effects from cholesterol-lowering statins “often are severe enough to allow patients to stop taking the drug. Of course, these side effects are accidental or psychosomatic disorders and have nothing to do with the drug.” “The previous clinical trials may have been funded by the pharmaceutical companies themselves, but “underestimated the side effects of statins.” The bottom line indicates that there is an urgent need to establish the true incidence of statin side effects.
“Is the percentage of symptomatic side effects in patients taking statins really caused by medication?” It is the title of a journal article that reports, even in a trial funded by Big Pharma, “only the small number of symptoms reported with statins are really due to statins,” and people taking statins may develop type 2 diabetes more than diabetes randomized to placebo sugar tablets. why? We are not yet sure exactly, but statins may have the effect of double insects in that they impair insulin secretion from the pancreas, while at the same time reducing the effectiveness of insulin by increasing insulin resistance.
Even the short-term use of statins can be “about twice as likely as diabetes and diabetic complications.” As shown below, my video should take statins at 1:49 in my video, fewer people develop diabetes and diabetes complications from statins for about five years than those who develop diabetes during statins. “More concerning, this increased risk has continued for at least five years since statin use stopped.”
“Considering the overwhelming benefits of statins in reducing cardiovascular events,” the number one murderer for men and women, is the increased risk of diabetes, our seventh major cause of death, increased by cardiovascular benefits? It’s a false dichotomy. There is no need to choose between heart disease and diabetes. Both causes can be dealt with the same diet and lifestyle changes. A diet that can not only stop heart disease, but also reverse it, is the same as that which can reverse type 2 diabetes. But what if, for some reason, you refuse to change your diet and lifestyle? If so, what are the risks and benefits of starting a statin? Don’t expect to get a full scoop from your doctor, as most people seemed ignorant about the causal relationship of statins with diabetes.
“Overall, for patients who are recommended by current guidelines, the benefits outweigh the risks,” but that’s what you decide. Before we can accurately quantify what the risks and benefits are, what are the recommendations in the current guidelines?
How should you determine whether a statin is right for you? “If you have a history of heart disease or stroke, we recommend taking statins without taking cholesterol levels into consideration.” period. Full stop. No discussion is necessary. The decision “if you don’t have a known cardiovascular disease yet” should be based on your own personal risk calculations. If you know your cholesterol and blood pressure count, you can easily do it online with the American Heart Disease Risk Estimator or Framingham Risk Profiler.
My favorite is the estimator at the American College of Cardiovascular Sciences. Because it poses you the risks of your current 10 years and your lifetime. So for people with a 5.8% risk of having a heart attack or stroke within the next decade, if they don’t clean up their actions, their lifelong risk will jump to 46%, which is almost the backbone of the coin. However, if they improve their cholesterol and blood pressure, my video could reduce that risk by 10 times or more to 3.9%, as shown below, at 4:11, as shown below.
Statin decisions are based on 10 years of risk, so what do you do with that number? Here, in my video, at 4:48, under current guidelines, if the 10-year risk is less than 5%, you should stick to dieting, exercise, smoking and reducing the number unless there is a situation where it is extended. In contrast, if the 10-year risk reaches 20%, the recommendation is to add statin medications in addition to making lifestyle changes. Unless there are any risk-enhancing factors, if the risk is below 7.5%, the tendency to stick to lifestyle changes is to move to adding drugs after 7.5%.
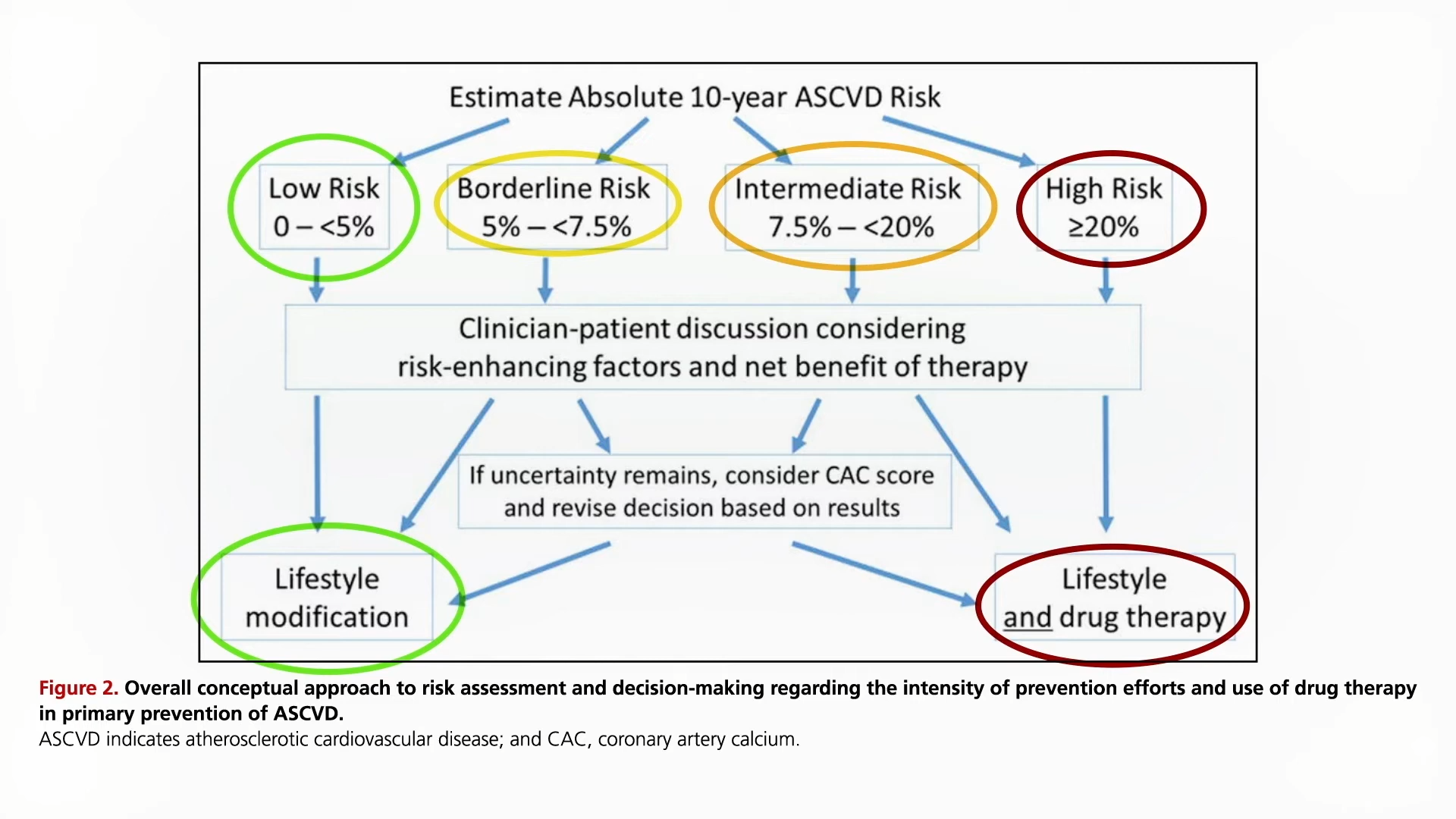
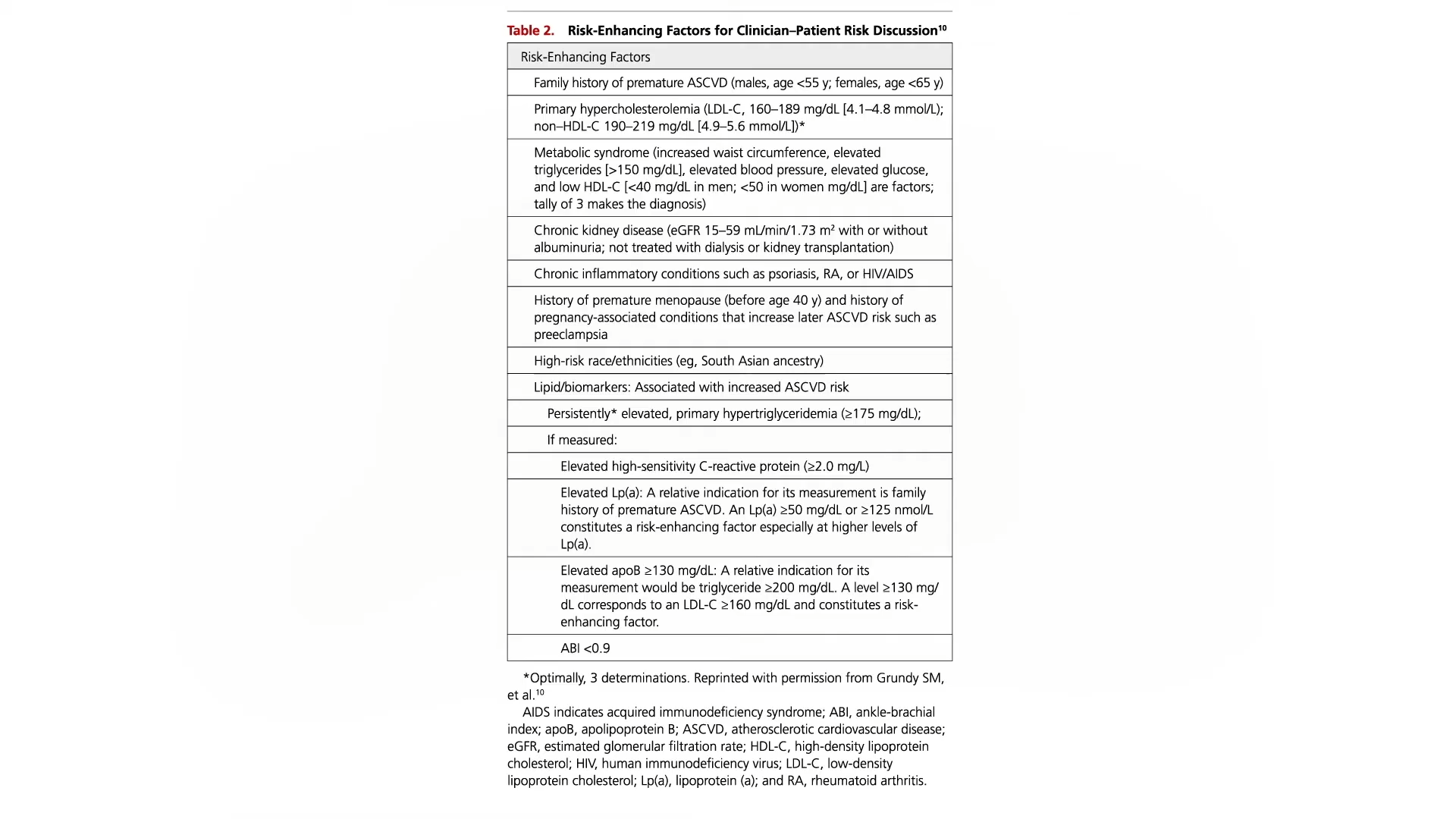
Risk-enhancing factors your physician should consider when making decisions include bad family history, truly high LDL cholesterol, metabolic syndrome, chronic kidney or inflammatory conditions, or persistently high triglycerides, C-reactive proteins, or LP(A). In my video, you can view the entire list here and at 4:54.
If still uncertain, the guidelines recommend considering obtaining a coronary calcium (CAC) score, but recently, despite relatively low radiation exposure from that test, the US Task Force on Preventive Services has explicitly concluded that current evidence is insufficient to conclude that it outweighs the harm.





